Osteoporosis
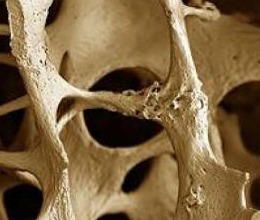 Osteoporosis, according to the WHO definition, is the “progressive systemic skeletal disease characterised by low bone mass and micro-architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture”.
Osteoporosis, according to the WHO definition, is the “progressive systemic skeletal disease characterised by low bone mass and micro-architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture”.
There are 2 components to osteoporosis (1) weak bones, resulting in (2) increased suseptibility to fractures.
Bone strength is dependent on 2 factors: (1) bone density and (2) bone quality. As there are currently no reliable methods of measuring bone quality, the diagnosis of osteoporosis tends to be made based on bone mineral density (BMD).
- "Although 80% of osteoporosis sufferers are women, as the longevity of the male population increases, the disease will assume increasing importance in men." ... Gro Harlem Brundtland
NATURAL HISTORY OF BONE LOSS
Bone density increases from birth through adolescence, reaching a peak in the twenties. Genetic, environmental and nutritional factors all play a role in contributing to the peak bone density achieved.
There is then slow, minimal decline in bone density from about 30 to 50 years. In men above 50 years, bone density declines at a rate of about 0.2 – 0.5% per year. In post-menopausal women, the rate of decline is significantly higher, at about 3-5% per year for about 5 – 8 years, then slows to about 1-2% per year thereafter.
RISK FACTORS
Many factors contribute to your overall risk of developing osteoporosis.
• Advanced age
• Female gender
• Caucasian or Asian race
• Thin and small body frame
• Positive family history of osteoporosis
• Personal history of fractures as an adult
• Excessive alcohol consumption
• Smoking
• Low dietary calcium
• Lack of exercise, in particular, weight-bearing exercise
• Malnutrition and poor general health
• Low estrogen states in women (eg. After menopause, removal or damage to ovaries)
• Low testosterone levels in men
• Chronic immobility
• Certain medical conditions eg. Hyperthyroidism, hyperparathyroidism, rheumatoid arthritis
• Certain medication eg. Heparin, phenytoin, corticosteroids
THE OSTEOPOROSIS SELF-TEST FOR ASIANS (OSTA) SCORE
In Asian women, the use of the OSTA Scoring system would help in the assessment of this risk.
Clinically, one can estimate the risk of osteoporosis by the OSTA scoring system. This is calculated as follows:
Age (in years) – Weight (in kg) = OSTA Score
Interpreting Results
|
OSTA
High > 20
|
Risk of osteoporosis is high (about 61%) |
|
OSTA
Moderate 1-20
|
Risk of osteoporosis is moderate (about 15%) |
|
OSTA
Low < 1
|
Risk of osteoporosis is low (about 3%) |
From the above, one observes that the older and lighter you are, the higher your risk. For example, if you are 40kg in weight, your OSTA score would be considered high once you are above 60 years old.
Based on your OSTA score and other risk factors, your doctor will advise you on whether you should proceed to do the DEXA scan to assess your Bone Mineral Density.
PREVALENCE
The estimated worldwide prevalence of osteoporosis in women is as follows:
• 50 – 59 years old, about 4%.
• 60 – 69 years old, about 8%
• 70 – 79 years old, about 25%
• 80 years and above, about 48%
In developed economies such as Singapore, the prevalence of osteoporosis is likely to increase as the population ages. In 2005, 1 in 12 was over 65 years. In 2030, 1 in 5 will be above 65 years.
EFFECTS OF OSTEOPOROSIS
Falls are more common among the elderly. A simple fall on weakened bones often results in fractures, and this most commonly occurs to the hip, vertebrae and wrists.
The statistics are grim. Up to 25% of patients do not survive beyond 1 year after a hip fracture. Of those who do, 20% become semi or fully dependent, and 40% experience some form of reduced mobility.
A person may otherwise be unaware that she/he has osteoporosis, until a fracture occurs. Pain then occurs at the site of fracture. If compression fractures occur in the spinal vertebrae, there may be backache with gradual loss of height and development of a "hunched" posture.
DIAGNOSIS
Bone strength is determined by both bone density and bone quality. As there are no reliable methods of measuring bone quality, the diagnosis of osteoporosis is made based on bone mineral density (BMD).
made based on bone mineral density (BMD).
About 80% of one's bone density is determined by one's genes, and the remaining 20% by lifestyle. Based on assessment of risk one's individualized risk for osteoporosis, your doctor will advise on the need for BMD testing.
The most common test for osteoporosis is the DEXA Scan (Dual X-ray Absorptiometry). It is the preferred technique for measuring BMD for the diagnosis of osteoporosis. The DEXA Scan is a painless, simple procedure, which is relatively easy to perform. The scanner produces 2 x-ray beams of different energy levels. The amount of x-rays that pass through the bone is measured for each beam, and the bone density is calculated based on the difference between the two beams.
DEXA scanning is typically done on the hip and spine, and bone density measured at these sites are taken as predictive of bone density of the skeleton in general.
MANAGEMENT
LIFESTYLE CHANGES
• Adequate intake of Calcium and Vitamin D
• Exercise – both weight-bearing and resistance training exercises have been shown to be effective in improving bone mineral density in women. Exercise also improves physical strength and postural stability, thus reducing risk of falls and further fractures.
• Avoid smoking and alcohol consumption – both are associated with increased risk of osteoporotic fractures.
• Fall prevention
TREATMENT
If your doctor has assessed that you require treatment, you may be started on the following medication. The choice of drug will depend on efficacy, ease of administration and cost, amongst other factors to be considered.
1. Bisphosphonates
2. Strontium ranelate
3. Raloxifene
4. Calcitonin
5. Teriparatide
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.
