Thyroid Disorders
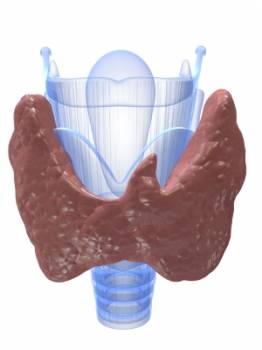 The thyroid gland is a small endocrine (hormone producing) gland situated in the neck, just below the Adam's apple. It has 2 halves, and is shaped somewhat like a butterfly. It is responsible for producing the thyroid hormone, a vital hormone for normal body function. Problems arise when there is under or over production of thyroid hormones by the thyroid gland, or the gland itself may grow abnormally, developing benign lumps or sometimes cancer.
The thyroid gland is a small endocrine (hormone producing) gland situated in the neck, just below the Adam's apple. It has 2 halves, and is shaped somewhat like a butterfly. It is responsible for producing the thyroid hormone, a vital hormone for normal body function. Problems arise when there is under or over production of thyroid hormones by the thyroid gland, or the gland itself may grow abnormally, developing benign lumps or sometimes cancer.
The hormones produced by the thyroid gland are Thyroxine (T4) and Triiodothyronine (T3).
These hormones are responsible for the following:
• Controlling Metabolism
• Controlling Growth and Development
REGULATION OF THE THYROID GLAND
The activity of the thyroid gland is tightly controlled by the normal functioning of the Hypothalmic-pituitary-thyroid axis. This axis is a team of 3 glands working in concert to ensure normal thyroid gland functioning. The hypothalamus is part of the brain, and it produces Thyrotropin Releasing Hormone (TRH), which stimulates the Pituitary gland (situated at the end of a stalk at the base of the brain) to produce the Thyroid Stimulating Hormone (TSH). It is this TSH which stimulates the Thyroid gland to produce the thyroid hormones T3 and T4.
The system works a little like a boiler and thermostat. The thyroid gland functions like the boiler which fires up to increase the metabolic rate of the body, whilst the hypothalamus functions like the thermostat, that controls the “temperature” of the “boiler”.
If thyroid hormone levels are too low, the thermostat senses this, and signals to the “boiler” (the thyroid gland) to produce more “heat” (thyroid hormone).
On the other hand, if thyroid hormone (“heat”) levels are sufficient, a negative feedback to the “thermostat” (the hypothalamus) causes it to produce less TRH. Lower TRH levels filter down to cause less thyroid hormone production.
WHAT CAN GO WRONG?
If something goes wrong with your thyroid gland, the changes may be very subtle initially, and symptoms may go largely unnoticed. Symptoms of hypothyroidism for instance, can easily be passed off as normal fatigue and lethargy.
Some Conditions of the Thyroid include:
(i) Hyperthyroidism (overactive thyroid gland)
(ii) Hypothyroidism (underactive thyroid gland)
(iii) Goitre (enlarged thyroid gland)
(iv) Thyroid cancer
HYPERTHYROIDISM - The Overactive Thyroid
Hyperthyroidism occurs when the thyroid gland produces excessive amounts of thyroid hormones into the blood stream.
Common symptoms include:
• Feeling hot and excessive sweating
• Tremors
• Palpitations
• Feeling of anxiety
• Increased appetite but loss of weight
• Hair loss
• Brittle nails
• Hyperactivity
• Swelling in the front of the neck (an enlarged thyroid gland is called a goitre)
• Eye problems: protruding eyes, watery eyes, visual disturbances, "bags" under the eyes.
Causes of Hyperthyroidism:
Graves Disease:
This is an autoimmune condition and is the most common cause of hyperthyroidism. It arises when the body's immune system mistakes normal thyroid tissue for foreign invaders, and starts attacking it.
Thyroid Nodules:
Lumps sometimes develop in the thyroid gland, and these lumps occasional become hyperactive, producing excessive amounts of thyroid hormone.
Excessive Amounts of Thyroid Hormone Replacement Therapy:
If one mistakenly takes too much thyroid hormone replacement medication (to treat hypothyroidism), the reverse may occur (hyperthyroidism).
Too Much Dietary Iodine:
A rare cause of hyperthyroidism.
Diagnosis of Hyperthyroidism:
Blood tests showing elevated thyroid hormone levels will confirm the diagnosis of hyperthyroidism. There will also be a correspondingly low level of TSH (see earlier explanation regarding this negative feedback relationship).
Sometimes, your doctor may order a radioactive iodine or technetium scan to obtain more information about the cause of your hyperthyroidism, as this may affect the type of treatment.
Treatment of Hyperthyroidism:
No treatment is perfect, and you will need to discuss the treatment options most suitable for you with your doctor. There are 3 forms of treatment for hyperthyroidism caused by Grave's disease.
(i) Drugs:
There are 2 antithyroid drugs used in the treatment of hyperthyroidism. They are: carbimazole (more commonly used), and propylthiouracil.
In general, higher doses are used initially and then are subsequently reduced in stages according to your response to treatment. This will mean regular visits to your doctor and regular blood tests. In general, symptoms start to improve after about 10 to 14 days of therapy.
Length of treatment may vary, but is commonly up till about 18 months. At the end of this period, you will be assessed by your doctor to see if you may stop your medication (more blood tests will be done to assess your risk of recurrence). After stopping medication, you will continue to be monitored for recurrence of hyperthyroidism. If your symptoms do recur, your doctor may offer you a second course of treatment with anti-thyroid drugs, or may discuss other treatment options with you.
What you should know about Anti-thyroid drugs:
In general, very few experience any side effects. The main concern is a very rare side effect in which the bone marrow is suppressed, causing neutropenia and agranulocytosis, which may occur at any time during treatment. Should you develop a sudden high fever with a severe sore throat, see your doctor immediately and tell him that you are on anti-thyroid medication. If a blood count confirms low white blood cell counts, the drug must be stopped immediately.
(ii) Radioactive Iodine:
Radioactive iodine is traditionally reserved for older patients and those who have completed having children. It is administered orally, and acts by destroying the thyroid cells which produce the thyroid hormones. Before you receive the dose of radioactive iodine, you will be given a consent form to sign, and will receive instructions about avoiding crowded areas and close contact with other people (especially children) for a period of a few days after therapy.
You will be asked to return to see your doctor on a regular basis to assess your thyroid function. The major side effect of radioiodine is the development of permanent hypothyroidism, requiring replacement therapy with thyroid hormones. Replacement therapy in hypothyroidism is generally deemed much better than anti-thyroid therapy (in hyperthyroidism), because the gland is dormant. This means less need for frequent monitoring of hormone levels, unlike in the treatment of hyperthyroidism, in which hormone levels may fluctuate ever so often.
(iii) Surgery:
Surgical removal of the thyroid gland is a treatment option for some patients. In experienced hands, results of surgery are generally good. However, your surgeon will inform you about some of the risks to consider regarding surgery:
• Small scar over the neck
• Small risk of damage to the parathyroid glands (which lie just behind the thyroid).
• Small risk of damage to the nerves supplying the voice box.
• Risk that you may not be euthyroid following surgery (that is, you may eventually become either hypothyroid or hyperthyroid)
HYPOTHYROIDISM - The Under-active Thyroid
Hypothyroidism occurs when the thyroid gland produces insufficient thyroid hormones, and when this happens, the body's functions slow down.
Common Symptoms Include:
• Fatigue and lethargy
• Feeling constantly cold
• Unexplained weight gain
• Depression and lack of concentration
• Slowed heart beat
• Hair loss
• Dry, thickened skin
• Puffy face with eye bags
• Flaking and pitting of the nails
Causes of Hypothyroidism:
• Hashimoto's Disease
This is an autoimmune condition which can lead to hypothyroidism.
• Thyroiditis
Thyroiditis refers to the inflammation of the thyroid gland from whatever cause (eg. Post-partum thyroiditis). Thyroiditis can lead to hypothyroidism.
• Thyroidectomy (Surgical removal of the thyroid gland)
Sometimes a large portion of the thyroid gland is removed, for instance in the treatment of thyroid cancer or Grave's disease, and the residual thyroid tissue is unable to produce sufficient thyroid hormones for normal body functioning.
• Radioiodine Therapy
Radioactive iodine is given to treat hyperthyroidism. Hypothyroidism usually results from this form of treatment.
• Certain Medication
Some medication such as lithium (for treatment of psychiatric disorders) and amiodarone (for treatment of abnormal heart rhythms), can sometimes cause hypothyroidism.
• Pituitary Gland or Hypothalamus Malfunction
If “up stream” stimulatory hormones (TRH and TSH) are not produced in sufficient quantities due to abnormal functioning of the pituitary gland or hypothalamus, then the thyroid gland will not produce sufficient thyroid hormones. There is usually an associated deficiency in other hormones as well, because the hypothalamus and pituitary gland are also involved in the control of many of these hormones.
• Lack of Dietary Iodine
This is a rare cause of hypothyroidism.
• Congenital Hypothyroidism
Diagnosis of Hypothyroidism:
Blood tests showing depressed thyroid hormone levels will confirm the diagnosis of hypothyroidism. There will also be a correspondingly high level of TSH (see earlier explanation regarding this negative feedback relationship).
Sometimes thyroid hormone levels (T3 and T4) are normal, but TSH levels are raised. This is a condition known as subclinical hypothyroidism, and it has been found that some of these patients go on to develop clinical hypothyroidism (in which thyroid hormone levels become depressed) with time.
Treatment of Hypothyroidism:
You will be offered thyroid hormone replacement therapy (thyroxine) by your doctor. In the initial period of starting replacement therapy, you will need to have your blood checked more regularly to see that TSH levels have returned to normal. Subsequently, you may only require annual checks when your condition becomes more stable.
Over the years, you may find that the dose of thyroid hormone you need goes up.
The Enlarged Thyroid
A goitre merely refers to an enlarged thyroid gland. It should be noted that goitres may produce normal levels of thyroid hormones (in which they are referred to as being 'euthyroid'), or abnormal levels of thyroid hormones (in which they may be either 'hyperthyroid' or 'hypothyroid').
1. Simple Diffuse Goitre
A simple diffuse goitre is seen as a symmetrical, painless, smooth swelling in the front of the neck, which moves up and down on swallowing. Most who develop these simple goitres are young women between the ages of 15 to 25 years of age. During pregnancy, these goitres may fluctuate in size.
2. Multinodular Goitre
Middle aged individuals usually present with multinodular goitres. In these goitres there are multiple small lumps within the thyroid gland, which may have arisen from a cyst, benign tumour (an adenoma), or rarely a malignant tumour. Multinodular goitres potentially become very large and may cause compression of the underlying structures, resulting in difficulty swallowing or even breathing.
3. Thyroid Nodules
Single nodules or lumps in the thyroid are also fairly common, and can occur at any age. These nodules may vary size, being as small as a pea, to as large as a golf ball. Sometimes, if bleeding occurs within the nodule, there may be sudden onset of pain. Asymptomatic nodules are also sometimes found on routine medical examination.
Investigating Enlarged Thyroid Glands
Blood Tests: to check if it is a euthyroid, hyperthyroid or hypothyroid gland.
Fine Needle Aspiration: a needle is inserted into a prominent thyroid nodule or cyst under local anaesthetic, to obtain thyroid cells for histological analysis. The appearance of the cells will help determine if the thyroid enlargement is a result of a benign growth or malignant tumour.
X-rays: X-rays are sometimes ordered to assess if there is compression of the trachea.
Ultrasound Scans: ultrasound scans are used to help assess the nature of the thyroid enlargement.
Isotope Scans: this is a radioisotope scan which helps determine if there are regions in the enlarged gland which are hyperactive.
Thyroid Cancer
Malignant tumours of the thyroid are extremely rare. These cancers are classified according to their histological appearance under a microscope. The main types seen are as follows:
Papillary thyroid cancer (the majority) - often occurring in young females. Prognosis is excellent.
Follicular thyroid cancer - usually occurring the older age groups.
Others - e.g. medullary thyroid cancer, anaplastic thyroid cancer, lymphoma, sarcoma, squamous cell carcinoma
Diagnosis of Thyroid Cancer
Thyroid cancers usually first present with either a thyroid nodule or enlarged lymph nodes in the neck region. Diagnosis is via histological testing of a fine needle aspirate.
Treatment of Thyroid Cancer
Cancers of the thyroid gland are generally treated by total or partial removal of the thyroid gland (thyroidectomy). This is usually followed-up by post-operative radioactive iodine to kill any remaining cancerous thyroid cells.
Radiotherapy may be used when the cancer is unresectable, when it recurs after surgery, or to relieve pain from bone spread (bone metastasis).
AUTOIMMUNE THYROID DISEASE
Our immune system serves to protect us from foreign invaders, such as bacteria and viruses. It recognizes these foreign invaders and produces specially tailored antibodies to combat them. In autoimmune diseases, however, the body's immune system mistakes normal, healthy body tissues, for foreign invaders. It produces antibodies directed at specific groups of tissue in the body, thereby destroying them.
There are, in general, 2 types of autoimmune thyroid disease:
(i) Grave's Disease (which causes hyperthyroidism) and
(ii) Hashimoto's Thyroiditis (which may cause transient hyperthyroidism, but eventually leads to hypothyroidism).
Other autoimmune conditions may co-exist. They include:
VITILIGO
The immune system attacks the pigment producing cells of the skin (melanocytes). This results in patches of skin with no pigmentation.
ALOPECIA
The immune system attacks the hair follicles, resulting in partial or complete hair loss.
TYPE I DIABETES
Type I diabetes, is also known as insulin-dependent, or juvenile-onset diabetes. It occurs when the immune system destroys the pancreatic cells responsible for insulin production.
PERNICIOUS ANAEMIA
In this condition, there is an autoimmune destruction of the gastric parietal cells, leading to the lack of intrinsic factor (a chemical secreted by the stomach cells). Since absorption of Vitamin B12 from the gut is dependent on this intrinsic factor, this condition leads to Vitamin B12 deficiency and a form of anemia (known as megaloblastic anemia) develops.
MYASTHENIA GRAVIS
This is an autoimmune neuromuscular disease characterized by fluctuating muscle weakness and fatiguability.
ADDISON'S DISEASE
Addison's disease is a rare condition in which the adrenal glands do not produce sufficient steroid hormones (glucocorticoids and often mineralocorticoids). One of the causes of Addison's disease is the autoimmune destruction of the adrenal cortex.
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.
