Gastroesophageal Reflux Disease
 Gastroesophageal Reflux Disease, also known as GERD for short, is a condition in which gastric juices flows up the oesophagus (the gullet), causing irritation of the oesophageal lining. It is this irritation of the oesophageal lining that produces the troublesome symptoms and complications of GERD.
Gastroesophageal Reflux Disease, also known as GERD for short, is a condition in which gastric juices flows up the oesophagus (the gullet), causing irritation of the oesophageal lining. It is this irritation of the oesophageal lining that produces the troublesome symptoms and complications of GERD.
The lower oesophageal sphincter (LES) is a ring of muscle at the bottom of the esophagus that acts like a valve between the esophagus and stomach. When the LES fails to close properly, acid from the stomach is allowed to flow up the oesophagus.
Symptoms Of GERD
The main symptoms of GERD in adults are:
(i) Heartburn: the burning-type sensation or pain felt in the chest which may rise to the throat.
(ii) Acid reflux/regurgitation: in which there is a sour or bitter taste in the back of the throat or mouth.
Other less common symptoms of GERD include increased salivation, chest pain, a persistent dry cough, asthma-like symptoms, difficulty swallowing, a persistent sore throat or hoarseness of voice.
Causes of GERD
As mentioned earlier, GERD is caused by the failure of the lower oesophageal sphincter to prevent reflux of stomach acid into the oesophagus.
Factors that contribute to GERD include:
• Hiatal hernia: a hiatal hernia occurs when the upper part of the stomach and the LES move above the level of the diaphragm. Normally, the diaphragm helps the LES function properly, but when a hiatal hernia is present, mechanical and motility factors come into play in increasing the likelihood of GERD occurring.
• Obesity: obesity is associated with GERD.
• Pregnancy
• Smoking
• Zollinger-Ellison syndrome
• Scleroderma and systemic sclerosis: which can affect normal oesophageal motility.
• Hypercalcaemia: which can increase gastrin production, thus increasing gastric acid production.
• Use of certain medication
Complications of GERD
Chronic GERD, if undetected or left untreated, can result in several potential complications. These would include the following:
• Reflux Oesophagitis - chronic irritation by gastric acid leads to inflammation and possible ulceration at the lower end of the oeophagus.
• Oesophageal Stricture - chronic inflammation and fibrosis can lead to stricture formation.
• Barrett's Oesophagus - chronic irritation by gastric acid causes the normal lining of the oesophagus to be replaced by a lining more like that of the stomach or intestine (change of the epithelial cells from squamous to intestinal columnar epithelium). The risk of oesophageal cancer is increased significantly in patients with Barrett's oesophagus.
Management of GERD
The management of GERD involves learning to avoid factors which can aggravate it, as well as medication or surgery (in severe cases).
Simply by avoiding factors that can make GERD worse, can help reduce the symptoms.
Lifestyle Modification
• If you smoke, stop.
• Avoid eating too close to bedtime. Leave at least 2-3 hours before bedtime for your last meal.
• Avoid large meals, specially for dinner or supper. Eat small, regular meals instead.
• Avoid lying down after meals.
• Sleep with the head end of your bed elevated. Place wood or cement blocks under the feet of your bed so that the head end is raised by six to nine inches. If this is not possible, wedges may be purchased from medical supply stores to elevate your body from the waist up. Raising your head with additional pillows has not been found to be effective.
• Lose weight if you are overweight.
• Avoid wearing tight clothing which may increase the pressure on your abdomen.
• Keep a food diary to help you see which foods tend to aggravate your GERD symptoms. By simply avoiding these food, you may find yourself having much fewer or less troubling symptoms.
 Foods to Avoid
Foods to Avoid
• Caffeine containing products eg. coffee, tea, colas
• Citrus fruits and juices
• Chocolate
• Fatty or fried foods
• Very spicy foods
• Garlic and onions
• Mint flavouring
Medication For GERD
Commonly used medication which your doctor may prescribe may include the following:
• Antacids - work by neutralising gastric acid.
• H2-blockers (histamine2-receptor antagonists) - work by blocking histamine's action and reduces acid production. Examples include famotidine, cimetidine and ranitidine.
• Proton Pump Inhibitors - these drugs act by blocking the action of acid pumps in the stomach. Proton pump inhibitors are more effective than H2 blockers, providing fast relieve of symptoms and heals the damage caused by acid in the oesophageal lining. Examples include omeprazole and esomeprazole.
• Prokinetic agents promote emptying of the stomach.
Investigations for GERD
 Occasional, if medication and lifestyle changes do not help relieve symptoms of GERD, then you may need to see a gastroenterologist or upper gastrointestinal surgeon. Certain tests or investigations may need to be carried out.
Occasional, if medication and lifestyle changes do not help relieve symptoms of GERD, then you may need to see a gastroenterologist or upper gastrointestinal surgeon. Certain tests or investigations may need to be carried out.
Barium Swallow: this is a radiographic examination in which you are made to drink a contrast solution and X-rays are taken. In a barium swallow, anatomical abnormalities show up well eg. hiatus hernia, strictures and ulcers. Inflammation or minor abrasions are not seen in a barium swallow.
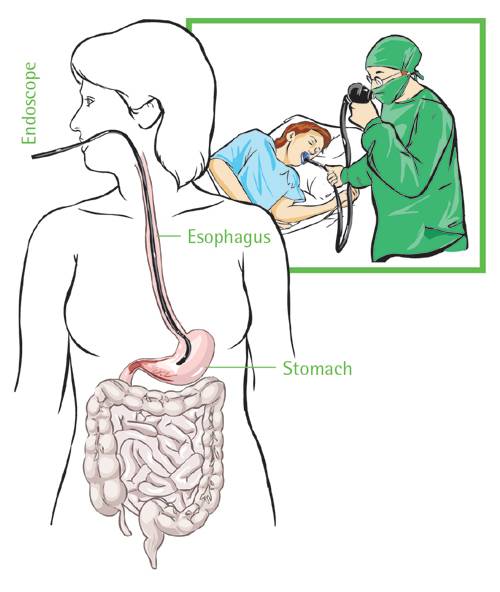
Gastroscopy: this allows for direct visualization of the oesophagus and stomach linings. Biopsies may be taken during the gastroscopic examination.
pH monitoring examination: a pH monitoring device is inserted into the oesophagus. As you go about your normal activities, this device measures when and how much acid is refluxed up your oesophagus. This measurement can be very useful when studied together with a carefully completed food diary, as this allows your doctor to see the correlation between what you eat/drink and your reflux episodes.
Surgery for GERD
Surgery is for GERD is sometimes done when lifestyle changes and medication do not help relieve GERD symptoms. Various types of surgery eg. Fundoplication, endoscopic techniques are performed, but they are beyond the scope of this article.
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.
