Liver Cancer
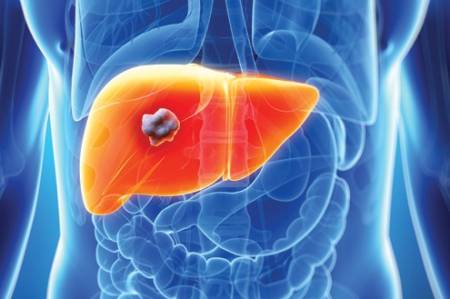 Primary liver cancer is a disease in which malignant (cancer) cells arise from tissues in the liver. The different types of primary liver cancer are usually named after the types of cells from which it is thought the cancer has developed. Hepatocellular carcinoma (HCC) or hepatoma arises from the main cells of the liver called hepatocytes and accounts for about 85% of primary liver cancers. A less common type of primary liver cancer originates from cells that line the bile duct called cholangiocytes and is therefore called cholangiocarcinoma or bile duct cancer.
Primary liver cancer is a disease in which malignant (cancer) cells arise from tissues in the liver. The different types of primary liver cancer are usually named after the types of cells from which it is thought the cancer has developed. Hepatocellular carcinoma (HCC) or hepatoma arises from the main cells of the liver called hepatocytes and accounts for about 85% of primary liver cancers. A less common type of primary liver cancer originates from cells that line the bile duct called cholangiocytes and is therefore called cholangiocarcinoma or bile duct cancer.
The liver is also the seat of another type of cancer called secondary (or metastatic) liver cancer. In this condition, the main cancer originates elsewhere in the body and secondary deposits are formed in the liver. A common example is colorectal cancer spreading to the liver via the bloodstream.
How Common Is Liver Cancer?
Worldwide, primary liver cancer is twice as common in men compared with women, and is the 5th and 7th most common cancer in males and females, respectively. Asian countries account for nearly 80% of the approximately 600000 cases of primary liver cancer diagnosed globally each year.
What Are The Risk Factors For Liver Cancer?
The three main risk factors for developing HCC (the most common primary liver cancer) are chronic hepatitis B infection, chronic hepatitis C infection and excessive alcohol consumption. The risk of an individual with chronic hepatitis B infection developing HCC is 100-fold that of an uninfected individual.
Other less common risk factors include aflatoxin (a poison found in mouldy peanuts, wheat, soya and grain), inherited conditions (eg. haemochromatosis, alpha-1 anti-trypsin deficiency) and any cause of cirrhosis (scarring throughout the liver) like autoimmune hepatitis or primary biliary cirrhosis. Many liver cancers can be prevented by public health measures that reduce exposure to these known risk factors.
Signs And Symptoms
Patients who develop HCC usually have no symptoms other than those related to their chronic liver disease. With worsening symptoms of the existing chronic liver disease like abdominal distension with fluid (ascites), encephalopathy (altered mental state), jaundice, or gastro-instestinal tract bleeding may heighten the suspicion of development of HCC. Besides that, some patients may have mild to moderate upper abdominal pain, weight loss, early satiety, lethargy, anorexia or a palpable mass in the upper abdomen.
Can We Screen For Liver Cancer?
Yes. Screening can help doctors find and treat HCC early, when the cancer is localized and more easily removed by surgery. This may in turn improve the chance of survival. Those with chronic hepatitis B infection and liver scarring (cirrhosis) due to hepatitis C or other causes are at increased risk and should be screened for liver cancer.
Screening involves:
• A blood test for alpha-fetoprotein (AFP) every 3-6 months
• An ultrasound scan of the liver every 6-12 months
Diagnosis & Assessment
How is Diagnosis made?
The following tests and procedures may be performed to diagnose HCC and to show the stage of the cancer:
• Physical examination for general signs of health. An examination of the abdomen will also be performed to check for hard lumps or ascites.
• Blood tests to check general health, liver function and the amount of AFP. The amount of AFP in the blood can be higher in people with HCC.
• A liver ultrasound scan that uses sound waves to produce a picture of the liver. This is a painless test and usually takes several minutes to perform. The picture may reveal a liver tumour.
• A computed tomography (CT) or magnetic resonance imaging (MRI) scan of the abdomen to visualize the three-dimensional picture of liver. It can show the size and position of a tumour, and whether it has spread.
Although a diagnosis of HCC can be made based on the amount of AFP in the blood and on dedicated CT or MRI scans, a liver biopsy may sometimes be needed to be sure of the diagnosis. If the cancer has not already spread and if there is a chance it can be removed, then a biopsy might not be performed. This is due to the small risk of the cancer spreading along the path of the needle when the biopsy needle is removed. In this situation, the diagnosis is confirmed after an operation to remove the tumour.
Treatment & Care
How Is Liver Cancer Treated?
The type of treatment for patients with HCC will depend on its stage (that is, its size and whether it has spread beyond its original site) and the patient’s general health. The main treatments used are surgery, tumour ablation, chemotherapy, targeted cancer therapy and radiotherapy.
Can Liver Cancer Be Prevented?
Yes. There are several things we can do to prevent liver cancer. These include:
1. Vaccinate against hepatitis B virus.
2. Avoid contact with known liver carcinogens, especially alcohol.
3. Avoid heavy meat and animal fat intake. Avoid mouldy peanuts and grains.
4. Go for regular screening if you are in the high risk group.
What kind of support is available?

CanHOPE, is a non-profit cancer counselling & support service initiated by Parkway Cancer Centre.
As part of the holistic approach towards cancer treatment, CanHOPE works closely with the medical & allied health professionals, offering a wide range of resources & information about cancer in helping patients & their caregivers to make effective, informed decisions in their treatment journey.
Join us in our support programmes that are available on a monthly basis.
CALL our CanHOPE counsellors: +65 67389333 or e-mail:
What Is Liver Cancer? originally appeared on Parkway Cancer Centre and has been republished with permission
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.

 Chemotherapy is the use of anti-cancer drugs to destroy cancer cells or stop them from dividing. It can help to control symptoms by shrinking the cancer and slowing its progression. Chemotherapy drugs are usually given as injections into the vein (intravenously), although they can sometimes be given as tablets. Chemotherapy may also be administered as part of a treatment called chemoembolisation. Chemoembolisation involves the injection of chemotherapy drugs directly into the cancer in the liver, together with a gel or tiny plastic beads to block blood flow to the cancer (embolisation). Not everyone is suitable for chemotherapy as it can only be given if the liver function is good enough.
Chemotherapy is the use of anti-cancer drugs to destroy cancer cells or stop them from dividing. It can help to control symptoms by shrinking the cancer and slowing its progression. Chemotherapy drugs are usually given as injections into the vein (intravenously), although they can sometimes be given as tablets. Chemotherapy may also be administered as part of a treatment called chemoembolisation. Chemoembolisation involves the injection of chemotherapy drugs directly into the cancer in the liver, together with a gel or tiny plastic beads to block blood flow to the cancer (embolisation). Not everyone is suitable for chemotherapy as it can only be given if the liver function is good enough.